Should the Global Community Be Concerned About the South African Variant?
Should the Global Community Be Concerned About the South African Variant?
February 23, 2021
Currently, the downward trend of SARS-CoV-2 infections per day in the U.S. is continuing, and the case numbers of COVID-19 are less than half of what it was at the peak of the pandemic (Worldometers).The mortality rate of COVID-19 is also beginning to decrease in the U.S., and similar trends are evident in many other countries as well. It’s not entirely clear what’s causing this downtrend in infection rates, though it may be related to increased compliance with preventive precautions. It is much too early to be due to vaccination and, in fact, the decrease is being observed in countries with a very low pace of vaccination or no vaccination. The new trend may also reflect, in part, natural immunity following up on large scale infection in some populations. However, the downtrend is likely a combination of all these parameters, yet no one definitively knows the cause. Viral-induced pandemics follow cyclic evolutions that we cannot control.
 New COVID-19 Variants
New COVID-19 Variants
While this new downtrend is good news, variants of concern originating from the UK, South Africa, Brazil and elsewhere are troubling. Vaccines generally provide protection against these variants, although efficacy is reduced against certain variants (see gvn.org/covid-19 for detailed information). Clearly, the virus is gradually evolving to adapt to our immune system. Thus, mass vaccination needs to be rapidly implemented to stop the spread of the variants. Eventually, we might need to develop more broadly effective vaccines or even pan-coronavirus vaccines.
B.1.351 (South Africa Variant)
The most concerning variant so far has emerged from South Africa (B.1.351 lineage; 501Y.V2). As with other variants, important questions include: 1) Is it more transmissible? 2) Is it more pathogenic? 3) Will vaccines be effective against it? and 4) Does prior infection with other SARS-CoV-2 confer protection against it? We’ll look at some of the early data that have bearing on these issues.
Clearly, the virus is gradually evolving to adapt to our immune system. Thus, mass vaccination needs to be rapidly implemented to stop the spread of the variants. Eventually, we might need to develop more broadly effective vaccines or even pan-coronavirus vaccines.
The Novavax vaccine, a full length spike protein contained in a lipid nanoparticle, was 90% effective in preventing symptomatic COVID-19 in UK, but only 49% effective in South Africa...Similarly, the Johnson and Johnson vaccine, a recombinant adenovirus, was 72% effective in the United States at protecting from moderate to severe disease, but only 57% in South Africa.
The recent variants are a serious concern, but the existing vaccines are still likely to be largely effective. However, the evolution of SARS-CoV-2 doesn’t stop here. It is possible that SARS-CoV-2 continues to circulate and evolve even after the mitigation of this pandemic. We might need an annual vaccination with updated vaccines similar to influenza vaccination.
The B1.351 variant was originally characterized by five non-synonymous signature mutations (D80A, D215G, E484K, N501Y and A701V) in the spike (S) protein, which were followed by the appearance of three others (L18F, K417N, and alternatively R246I or a small deletion at the same site)(1). In addition, there are other characteristic mutations besides those in the spike protein. An increase in transmissibility was inferred from the rapidity at which B1.351 displaced previous viral genotypes. Specifically, this variant was first detected in Nelson Mandela Bay, South Africa, in early October 2020. Within weeks, it became the dominant virus in parts of the country. Currently, the variant has been detected in more than 90% of sequenced samples from COVID-19 patients in South Africa. Further, the variant has already spread to more than 30 countries. Although the variant is fast-spreading, its impact on severity has not been demonstrated by testing in an animal model system. Obviously, however, even if a variant does not enhance disease severity, greater transmissibility consequently results in an increase in cases of COVID-19, hospitalization, and eventually mortality.
 Spike Protein Vaccines
Spike Protein Vaccines
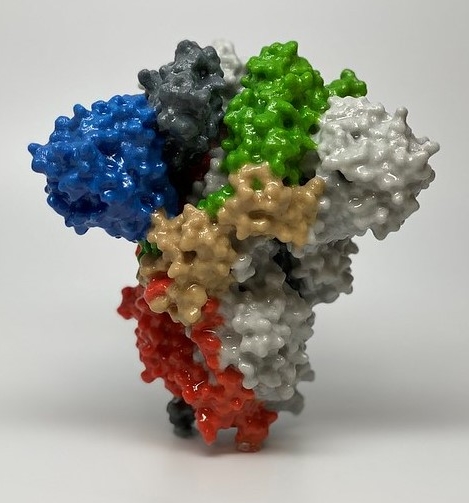
Most COVID-19 vaccines are using the spike protein as a major immunogen. Given the number of mutations in the B.1.351 spike protein, it is easy to understand why there are concerns regarding vaccine efficacy. There are several ways to investigate this. The quickest way to gain some insight is to determine whether antibodies elicited by the vaccines can recognize or neutralize the virus, using either protein binding studies or virus neutralization tests in vitro. The former simply measures recognition and not neutralization. The latter tests actual neutralization of SARS-CoV-2 using infectious virus in a biosafety level 3 facilities or pseudotypes of the virus bearing the SARS-CoV-2 spike protein in a biosafety level 2. A surrogate neutralization assay has also been developed(2) which does not require using the virus. None of these methods, however, take into account T cell activity, antibody-dependent cytotoxicity, or the induction of innate immunity, which are likely important factors for protective efficacy of vaccines.
Neutralization
Wang et al.(3) researched antibodies and memory B cells from people who were vaccinated with either the Moderna or the Pfizer mRNA vaccines. Both vaccines induced similar pseudotype plasma neutralizing activity to each other of prototypical SARS-CoV-2, and similar to that of 1.3 months post-infection convalescent plasma. Neutralizing titers correlated well with antibody binding activity to the S protein and the receptor binding domain (RBD). The ability of vaccinee plasma to neutralize B1.351 was assessed using pseudotypes containing one or all of three mutation in the B1.351 S protein (K417N, E484K and N501Y). Neutralizing activity against these viruses was reduced from 1- to 3-fold. Monoclonal antibodies (MoAbs) against the RBD were obtained from individual memory B cells. About 25% of 84 RBD MoAbs showed at least 5-fold reduced binding to the mutated RBDs. 9/17 MoAbs were 10-fold less effective in pseudotype neutralization against the E484K mutant, 4-fold against K417N, and 4-fold against N501Y. Wu et al.(4) also looked at sera from Moderna vaccines for neutralizing titers in pseudovirus assays. They compared the ability to neutralize pseudoviruses with a spike protein containing the D614G mutation (5), with the ability to neutralize pseudoviruses containing K417N, E484K, and N501Y, or the full complement of B.1.351 mutations. There was a reduction in geometric mean neutralizing titers of around 3- to 6-fold, observations generally congruent with those of Wang et al.(3). It should be noted, however, that titers were still high against the variants (1/290), suggesting that reasonably robust protection has been retained. Jangra et al.(6) reported that the E484K mutation alone reduced the neutralization efficiency of sera from people vaccinated with the Pfizer vaccine about 3-fold, although again neutralization occurred.
 Vaccines and the South Africa Variant
Vaccines and the South Africa Variant
As noted above, none of these studies take into account T cell activity (or the role of antibody-dependent cytotoxicity). In addition, the level of neutralizing activity required for protection is unclear. Therefore, these in vitro studies cannot provide correct answers for the protective efficacy of vaccines against this variant. Several studies from vaccine clinical trials suggest that current vaccines will be somewhat less effective against the South African variant. The Novavax vaccine, a full length spike protein contained in a lipid nanoparticle, was 90% effective in preventing symptomatic COVID-19 in UK, but only 49% effective in South Africa. There are some caveats, however. The identity of the breakthrough viruses was not established by sequencing. Also, the prevalence of HIV-1 in South Africa could have influenced efficacy. Indeed, protection in people without HIV-1 was greater (60%). And even 50-60% will be quite helpful for combating the epidemic. Similarly, the Johnson and Johnson vaccine, a recombinant adenovirus, was 72% effective in the United States at protecting from moderate to severe disease, but only 57% in South Africa. These two studies suggest a somewhat reduced efficacy against B.1.351. Yet, and most important, these studies have demonstrated that besides the contamination rate such vaccines have protected against developing severe COVID-19 and this is a major achievement.
More challenging news was that the AstraZeneca vaccine, another recombinant adenovirus, has only offered poor protection against mild or moderate illness in young healthy volunteers in South Africa, leading the health authorities to halt the trials in the country. Currently, scientists are reevaluating the data to reconsider the vaccination against more severe cases of COVID-19. Overall, it is fair to say that there is much to be learned. Clearly, we will need vaccination to proceed with all due speed, and we will ultimately need more broadly effective vaccines and alternatively, pan-coronavirus vaccines.
Reinfection
What about protection acquired by previous infection with non-B.1.351 variants? Infection presumably would induce a broader immune response than would vaccines containing a single viral protein. On the other hand, infection appears to result in a weaker neutralizing response than does vaccination. Indeed, Jangra et al.(6) found that sera with lower neutralizing titers from previously infected people lacked neutralizing ability against B.1.351 entirely. A more direct answer as to how well prior infection protects against reinfection with B.1.351 comes from the Novavax vaccine trials in South Africa. In the placebo arm of the trials, prior infection did not appear to provide protection against B.1.351since there was no difference in the infection rate between previously infected and not previously infected people. As mentioned above, however, the vaccine was 50-60% protective. Anecdotally, recently a 58-year-old immunocompetent male who experienced a mild case of COVID-19 became critically ill 4 months later. Sequencing confirmed the presence of B.1.351(7). A similar case was reported in Israel in the case of a man who had traveled to Turkey. However, the disease in this case was mild. More recently, the number of Israelis reinfected with B.1.351 has increased, thus increasing concerns over the new variant.
Conclusion
Certainly, as for any virus, SARS-CoV-2 is evolving to adapt to humans. The recent variants are a serious concern, but the existing vaccines are still likely to be largely effective. However, the evolution of SARS-CoV-2 doesn’t stop here. It is possible that SARS-CoV-2 continues to circulate and evolve even after the mitigation of this pandemic. We might need an annual vaccination with updated vaccines similar to influenza vaccination. Ultimately, development of pan-coronavirus vaccines is an important strategy in preparing for future pandemics.
- H. Tegally et al., Emergence and rapid spread of a new severe acute respiratory syndrome-related coronavirus 2 (SARS-CoV-2) lineage with multiple spike mutations in South Africa. medRxiv, 2020.2012.2021.20248640 (2020).
- C. W. Tan et al., A SARS-CoV-2 surrogate virus neutralization test based on antibody-mediated blockage of ACE2-spike protein-protein interaction. Nat Biotechnol 38, 1073-1078 (2020).
- Z. Wang et al., mRNA vaccine-elicited antibodies to SARS-CoV-2 and circulating variants. bioRxiv, 2021.2001.2015.426911 (2021).
- K. Wu et al., mRNA-1273 vaccine induces neutralizing antibodies against spike mutants from global SARS-CoV-2 variants. bioRxiv, (2021).
- B. Korber et al., Tracking Changes in SARS-CoV-2 Spike: Evidence that D614G Increases Infectivity of the COVID-19 Virus. Cell 182, 812-827 e819 (2020).
- S. Jangra et al., The E484K mutation in the SARS-CoV-2 spike protein reduces but does not abolish neutralizing activity of human convalescent and post-vaccination sera. medRxiv, (2021).
- N. Zucman, F. Uhel, D. Descamps, D. Roux, J.-D. Ricard, Severe reinfection with South African SARS-CoV-2 variant 501Y.V2: A case report. Clinical Infectious Diseases, (2021).
