Exploring the Mystery of Acute Pediatric Non-A-E Hepatitis
Recent outbreaks of non-A, -B, -C, -D, or -E hepatitis among young children have presented epidemiologists with a mystery. The hepatitis cases tended to be severe, leading in many cases to liver transplantation. But, in searching for an infectious origin, one group of researchers detected in many of these hepatitis cases a prominent cause of diarrhea-associated mortality, adenovirus type 41 (HAdV-41) (1), which suggests one possible causal association. More recently, however, other researchers reported a tight association between these hepatitis cases and the presence of adeno-associated virus type 2 (AAV2) in blood, liver, and stool (2-4), suggesting another possible causal association. Moreover, the second group of researchers reported a close genetic association with a class II MHC allele (HLA-DRB1*04:01); 12 of 13 cases were positive (2, 3). Using Polymerase Chain Reaction (PCR) to analyze wastewater, still another team of researchers found a geographic association between pediatric hepatitis and both HAdV-41 and AAV2 (5). Taken together with an abundance of T-cells in affected livers, a dysregulated antiviral immune response may be involved in these acute pediatric hepatitis cases.
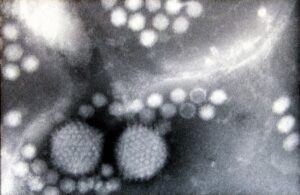 To better understand the situation, it is important to consider AAV2 in more detail. AAV was originally discovered as an adventitious presence in HAdV cultures. AAVs are small non-enveloped viruses with a single stranded genome of ~4.8 kilobases. They lack sufficient genes for replication and must therefore rely on helper viruses for propagation. HAdVs serve as helper viruses, as do several herpesviruses, including HHV-6. Notably, there’s also an association of pediatric hepatitis with HHV-6 (4). AAV can integrate into human DNA at a specific site on chromosome 19. This unusual predictability, along with the ability to infect non-dividing cells, has made AAV a popular candidate for gene therapy. However, the ability of AAV2 to integrate into host cell DNA is potentially a double-edged sword: Integration of Hepatitis B Virus genome contributes to liver carcinogenesis and it is plausible that AAV2 genome insertion might also lead in rare instances to hepatocellular carcinomas, generally in the absence of cirrhosis, by insertional mutagenesis (6). Indeed, it has been demonstrated that some AAV2 clonal insertions can induce expression of several cancer-related genes including cyclins and telomerase; thus, the nature of the mutated genes along with the clonality of the insertions leads to the suggestion that these viral integrations may contribute to carcinogenesis.
To better understand the situation, it is important to consider AAV2 in more detail. AAV was originally discovered as an adventitious presence in HAdV cultures. AAVs are small non-enveloped viruses with a single stranded genome of ~4.8 kilobases. They lack sufficient genes for replication and must therefore rely on helper viruses for propagation. HAdVs serve as helper viruses, as do several herpesviruses, including HHV-6. Notably, there’s also an association of pediatric hepatitis with HHV-6 (4). AAV can integrate into human DNA at a specific site on chromosome 19. This unusual predictability, along with the ability to infect non-dividing cells, has made AAV a popular candidate for gene therapy. However, the ability of AAV2 to integrate into host cell DNA is potentially a double-edged sword: Integration of Hepatitis B Virus genome contributes to liver carcinogenesis and it is plausible that AAV2 genome insertion might also lead in rare instances to hepatocellular carcinomas, generally in the absence of cirrhosis, by insertional mutagenesis (6). Indeed, it has been demonstrated that some AAV2 clonal insertions can induce expression of several cancer-related genes including cyclins and telomerase; thus, the nature of the mutated genes along with the clonality of the insertions leads to the suggestion that these viral integrations may contribute to carcinogenesis.
Among the cellular tropism of AAVs are hepatocytes (7), the major functional cells of the liver. AAV, however, has not previously been associated with any diseases (8). Thus, the close association with pediatric hepatitis is surprising. But, taking together both the presence of immune cells in the liver of hepatitis cases and the apparent DRB1*04:01 specificity, the mechanism behind the acute hepatitis—if the association with AAV2 and/or HAdV-41 is indeed causative—is likely dysregulated antiviral immunity. Humoral immunity to AAV2 includes neutralizing antibodies and their prevalence is high in human populations (9). AAV2 also elicits cell-mediated immunity. It is not well studied but includes a cytotoxic T-cell response to the AAV capsid protein (10).

Although cases of pediatric hepatitis are closely associated with AAV2 helper viruses (HAdV41, HHV-6), there don’t seem to be data to their direct contribution to the disease, either for the helper viruses or for AAV2 itself. Could the important contributory factor be their immunostimulatory properties? Or could they facilitate replication of AAV2 to a level that leads to immune over-stimulation? Or is their presence simply a statistical anomaly? Clearly much further study is needed to understand the etiology of pediatric hepatitis and the mechanisms are likely to be complex.
This situation points to a central issue in virus-induced diseases: the extent to which these disease manifestations are due directly to viral activity versus the host immune responses to infection. These responses can include over-exuberant inflammation or autoimmunity, perhaps due to molecular mimicry of host proteins by viral proteins. A further complication is that many viruses encode genes that cause immune dysregulation as a means to evade the host immune response, as is the case with Covid and SARS-CoV2. Certainly, there is still much to learn about the causal mechanisms of pediatric hepatitis, with particular focus on host immune responses, just as there is still much to learn regarding many other virus-associated diseases, too.
- R. Elsheikh et al., Acute hepatitis of unknown origin in children: Behind the statistics. Hepatology, (2022).
- A. Ho et al., Adeno-associated virus 2 infection in children with non-A-E hepatitis. Nature, (2023).
- S. Morfopoulou et al., Genomic investigations of unexplained acute hepatitis in children. Nature, 1-13 (2023).
- V. Servellita et al., Adeno-associated virus type 2 in US children with acute severe hepatitis. Nature, 1-7 (2023).
- N. A. Martin et al., Adeno-Associated Virus 2 and Human Adenovirus F41 in Wastewater during Outbreak of Severe Acute Hepatitis in Children, Ireland. Emerg Infect Dis 29, 751-760 (2023).
- J. C. Nault et al., Recurrent AAV2-related insertional mutagenesis in human hepatocellular carcinomas. Nat Genet 47, 1187-1193 (2015).
- D. D. Koeberl, I. E. Alexander, C. L. Halbert, D. W. Russell, A. D. Miller, Persistent expression of human clotting factor IX from mouse liver after intravenous injection of adeno-associated virus vectors. Proc Natl Acad Sci U S A 94, 1426-1431 (1997).
- N. R. Blaeklow, in Parvoviruses and human disease. (CRC Press, 2018), pp. 165-174.
- R. Calcedo, L. H. Vandenberghe, G. Gao, J. Lin, J. M. Wilson, Worldwide epidemiology of neutralizing antibodies to adeno-associated viruses. J Infect Dis 199, 381-390 (2009).
- D. E. Sabatino et al., Identification of mouse AAV capsid-specific CD8+ T cell epitopes. Mol Ther 12, 1023-1033 (2005).
