Emergence and Global Spread of SARS-CoV-2 Variants
Emergence and Global Spread of SARS-CoV-2 Variants
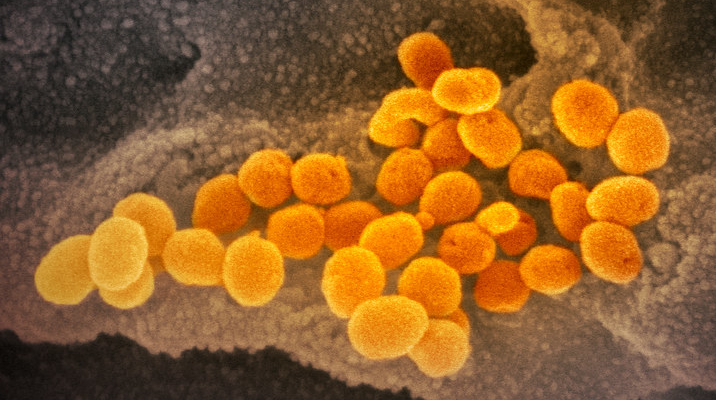
With the extended COVID-19 pandemic, SARS-CoV-2 is evolving, and multiple COVID-19 variants are circulating globally. Since December, 2020, a great deal of attention has been focused on emergence of SARS-CoV-2 variants from the UK (VOC 202012/01; B1.1.7. lineage) and from South Africa (20C/501Y.V2; B.1.351 lineage). In the UK, a new variant emerged with an unusually large number of mutations and has spread rapidly in the UK. In September, 2020, this variant represented just one in four new diagnoses of COVID-19, whereas by mid-December, this had increased to almost two thirds of new cases in London (1). Currently, the variant has been detected in at least 41 different countries. The South African variant was first detected in the Nelson Mandela Bay metropolitan area of the Eastern Cape province of South Africa (2). As the variant spreads faster than other earlier variants of the virus, the variant may be driving the second wave of the pandemic in the country. Preliminary epidemiologic, modelling, phylogenetic and clinical findings suggest that the variants have increased transmissibility.
D614G Mutation
The current situation is reminiscent of the emergence of a previous variant with a mutation in the spike protein, D614G. Based upon rapid prevalence increases, it was suspected of being more contagious (although not more pathogenic) (3). Notably, people infected with D614G had higher levels of viral RNA in their upper respiratory tract than those with original virus, although its titers in the lower respiratory tract remained indifferent between the two viruses (4). D614G has since become the predominant variant worldwide, supporting the earlier speculation about enhanced transmissibility.
New Variants
B1.1.7, the UK lineage, is defined by the presence of a range of 14 mutations resulting in amino acid changes and three deletions (David Ostrov, University of Florida (personal communication). Nine of the non-synonymous mutations are located in the spike (S) protein. Importantly, N501Y mutation in the receptor-binding domain (RBD) is predicted to enhance binding to the ACE2 receptor. Three, A570D, D614G and S982A, may affect cleavage and fusion dynamics. 69/70 deletion likely leads to a conformational change in the spike protein. P681H mutation locates near the S1/S2 furin cleavage site and could alter S1/S2 cleavage in endosomes Thus, these changes could potentially affect cell infectivity and replication of virus. Beside spike protein, a mutation of Q27stop causes truncation and likely loss of function of ORF8 (studies here and here). Wild type ORF8 suppresses type 1 interferon responses so loss of ORF8 function could lead to milder disease. B.1.351, the South Africa lineage, contains N501Y as well as K417N and E484K in the RBD of S protein, which can enhance binding to the ACE2 receptor. Interestingly, two of these mutations, E484K and N501Y, are within the receptor-binding motif (RBM) of the RBD. The E484K mutation has been shown to reduce antibody recognition.
Mutations and Diagnostics, Therapeutics, and Vaccines
 How these mutations can affect currently available diagnostics, therapeutics, and vaccines? In particular, a mass vaccination approach has been applied in several countries to curb the pandemic. To answer its effect on the efficacy of vaccines, a study evaluated ability of sera from vaccinees who had received the Pfizer vaccine to neutralize isogenic virus containing either N501 or the variants Y501. This study found equivalent neutralization titers against wild type and mutant viruses, thus confirming the effectiveness of current vaccine against this variant (5). The front-runner vaccine companies, Pfizer and Moderna, have confirmed that their vaccines can be effective against these variants. However, it needs to be evaluated by using live viruses of variants. As noted above, the N501Y substitution in an otherwise isogenic backbone is not sufficient to adversely affect neutralization by vaccinee serum, at least with the Pfizer vaccine. It seems intuitive that this would hold for the other vaccines. However, this result does not take into account the other spike protein mutations in B1.1.7, the UK lineage, and/or the possible alterations in T cell epitopes, so a somewhat open question remains. It is possible that these mutations (notably, E484K) could reduce vaccine efficiency to some degree (6). In particular, E484K mutation has been also detected in a new variant lineage, B1.1.28, from Brazil (7). This brings concern to vaccination programs. Effect of E484K mutation on immune evasion and reinfection is currently characterized by using convalescent sera. Since the vaccines are designed to elicit robust levels of neutralizing antibodies and other T-cell immunity, these minor changes may not greatly reduce protective efficacy of vaccines. However, it needs to be evaluated by using live viruses of variants. Importantly, it should also stimulate efforts to discover more broadly reactive vaccines not only against SARS-CoV-2 but also against future emerging coronaviruses.
How these mutations can affect currently available diagnostics, therapeutics, and vaccines? In particular, a mass vaccination approach has been applied in several countries to curb the pandemic. To answer its effect on the efficacy of vaccines, a study evaluated ability of sera from vaccinees who had received the Pfizer vaccine to neutralize isogenic virus containing either N501 or the variants Y501. This study found equivalent neutralization titers against wild type and mutant viruses, thus confirming the effectiveness of current vaccine against this variant (5). The front-runner vaccine companies, Pfizer and Moderna, have confirmed that their vaccines can be effective against these variants. However, it needs to be evaluated by using live viruses of variants. As noted above, the N501Y substitution in an otherwise isogenic backbone is not sufficient to adversely affect neutralization by vaccinee serum, at least with the Pfizer vaccine. It seems intuitive that this would hold for the other vaccines. However, this result does not take into account the other spike protein mutations in B1.1.7, the UK lineage, and/or the possible alterations in T cell epitopes, so a somewhat open question remains. It is possible that these mutations (notably, E484K) could reduce vaccine efficiency to some degree (6). In particular, E484K mutation has been also detected in a new variant lineage, B1.1.28, from Brazil (7). This brings concern to vaccination programs. Effect of E484K mutation on immune evasion and reinfection is currently characterized by using convalescent sera. Since the vaccines are designed to elicit robust levels of neutralizing antibodies and other T-cell immunity, these minor changes may not greatly reduce protective efficacy of vaccines. However, it needs to be evaluated by using live viruses of variants. Importantly, it should also stimulate efforts to discover more broadly reactive vaccines not only against SARS-CoV-2 but also against future emerging coronaviruses.
Could the changes in variants affect nucleic acid-based tests? The answer seems to be yes depending on the assay system. In a TaqPath multiplex RT-PCR assay targeting amplification of the ORF1ab, the N gene, and the S gene, amplification of the ORF1ab and N genes were successful, but detection of the N1.1.7 S gene was failed (8). This is important for two reasons. First, the phenomenon, called S dropout, allows discrimination of the new variant from other strains. Secondly, it raises the risk of RT-PCR assay for diagnostic of COVID-19 with the variants. A recent report describes PCR primer sets that are nearly 100% effective with N1.1.7.7 S gene amplification (9).
The front-runner vaccine companies, Pfizer and Moderna, have confirmed that their vaccines can be effective against these variants.
Could the changes in variants affect nucleic acid-based tests? The answer seems to be yes depending on the assay system.
These variants likewise do not thus far seem to be more pathogenic, while the higher titers in the upper tract may also reflect higher transmissibility.
Conclusion
The big question is, of course, whether these mutations increased viral transmissibility and pathogenicity. The earliest indications of increased transmissibility have been inferential and come from genomic studies that show it rapidly becoming dominant in places where it is introduced. This is of course circumstantial, although it should be noted that this was also the indication for D614G, which in fact did prove more infectious. A recent study used the S dropout phenomenon to compare viral titers in nasal swabs. 35% of people infected with N1.1.7, as identified by the inability to amplify the S gene, had viral RNA titers of between 10 and 10,000-fold greater than 1×106, compared to only 10% of those infected with non-B1.1.7, the UK lineage, viruses (10). This may be similar to the situation with D614G, in which there are much higher titers of viral RNA in the upper respiratory tract, although titers in the lower respiratory tract are normal (3). This may explain why D614G is more transmissible but not more pathogenic. These variants likewise do not thus far seem to be more pathogenic, while the higher titers in the upper tract may also reflect higher transmissibility. Other contributory mechanisms may include a higher affinity for its receptor, as described above. Interestingly, a mouse-adapted virus acquired N501Y mutation. Can this specific mutation change the viral tropism, thus leading to the spread of variants to mice and causing reverse zoonotic? Either way, even if the variants are not more pathogenic, their increased transmissibility alone would still lead to increased hospitalization and mortality. It will be critical to enhance the capacity of genetic surveillance for early detection of emerging variants and to share the data through well-established database system (i.e., GISAID) and international health organizations.
- Kirby, T. New variant of SARS-CoV-2 in UK causes surge of COVID-19. Lancet DOI:https://doi.org/10.1016/S2213-2600(21)00005-9
- Emerging SARS-CoV-2 Variants. Available at: https://www.cdc.gov/coronavirus/2019-ncov/more/science-and-research/scientific-brief-emerging-variants.html.
- Korber et al., Tracking Changes in SARS-CoV-2 Spike: Evidence that D614G Increases Infectivity of the COVID-19 Virus. Cell 182, 812-827 e819 (2020).
- Lorenzo-Redondo et al., A Unique Clade of SARS-CoV-2 Viruses is Associated with Lower Viral Loads in Patient Upper Airways. medRxiv, (2020).
- Xie et al., Neutralization of N501Y mutant SARS-CoV-2 by BNT162b2 vaccine-elicited sera. bioRxiv, 2021.2001.2007.425740 (2021).
- J. Greaney et al., Comprehensive mapping of mutations to the SARS-CoV-2 receptor-binding domain that affect recognition by polyclonal human serum antibodies. bioRxiv, 2020.2012.2031.425021 (2021).
- M. Voloch et al., Genomic characterization of a novel SARS-CoV-2 lineage from Rio de Janeiro, Brazil. medRxiv, 2020.2012.2023.20248598 (2020).
- Kidd et al., S-variant SARS-CoV-2 is associated with significantly higher viral loads in samples tested by ThermoFisher TaqPath RT-QPCR. medRxiv, 2020.2012.2024.20248834 (2020).
- Lopez-Rincon et al., Design of Specific Primer Set for Detection of B.1.1.7 SARS-CoV-2 Variant using Deep Learning. bioRxiv, 2020.2012.2029.424715 (2020).
- Gu et al., Adaptation of SARS-CoV-2 in BALB/c mice for testing vaccine efficacy. Science 369, 1603-1607 (2020).
