Correlates of Protection
Role of Correlates of Protection, or Immune Measurements, in Predicting Protective Immunity of COVID-19 Vaccines
March 29, 2021
Broadly speaking, correlates of protection are measurements of immune parameters that allow prediction of the degree of protection against infection or disease induced by a pathogen. A prime point of interest in consideration of protection against SARS-CoV-2 and COVID-19 is: what are the relevant correlates of protection? These, unfortunately, are not yet completely understood. Firstly, protection could mean protection from detectable infection (also known as sterilizing immunity), protection from symptomatic infection, or protection from severe disease. Secondly, it is likely that there is not only one protective mechanism, but that components of innate, B-cell and T-cell immunities can synergistically play important roles in protection. Correlates of protection and their induction and durability will need to be understood to effectively open society in the post-vaccination stage of the pandemic.
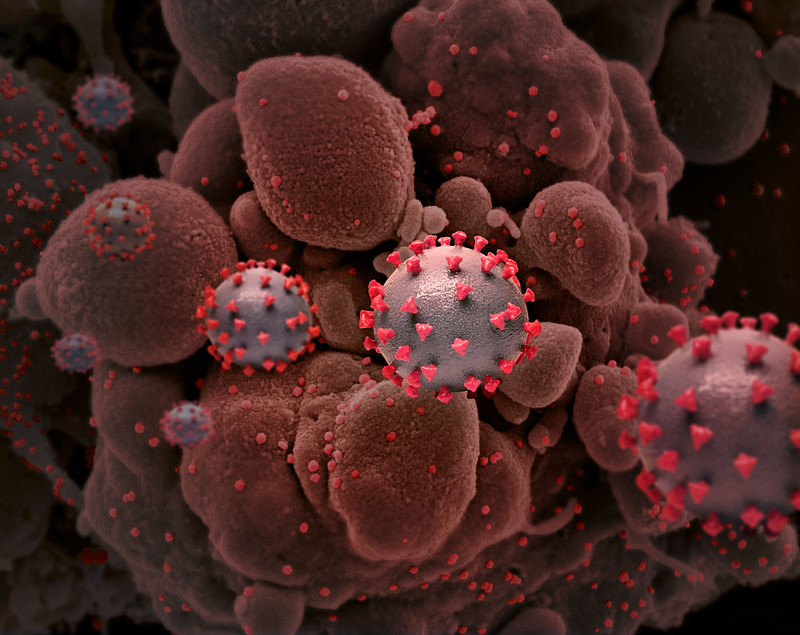 The protective mechanisms resulting from natural infection likely differ in part from those induced by vaccination. Induction of immune responses by natural infection involves all the viral proteins, but modern vaccine technology mostly focuses on the viral surface protein (i.e., spike protein in the case of COVID-19 vaccine). Indeed, the spike is a good target for CD4+ T cell, T follicular helper (Tfh) cell, and CD8+ T cell responses in SARS-CoV-2-infected people. Correlates of protection are generally established by comparative immunological assays or studies. One of the simplest examples is from studies using neutralizing monoclonal antibodies (nMAbs). Administration of either of two human nMAbs provided rhesus macaques with sterilizing immunity to challenge(1). When administered to humans early in infection, nMAbs help prevent progression to serious disease, indicating that neutralizing antibodies are likely to be a correlate of protection. Paradoxically, however, people with severe disease tend to have very high levels of neutralizing antibodies, so it may be that the timing of the presence of sufficient antibodies is important or that the types of neutralizing antibodies matter. And, it is important to remember that a correlate of protection does not mean that the measured parameter is the sole cause of protection. Correlation is not causation. Obviously, additional complex immune mechanisms are required for protection.
The protective mechanisms resulting from natural infection likely differ in part from those induced by vaccination. Induction of immune responses by natural infection involves all the viral proteins, but modern vaccine technology mostly focuses on the viral surface protein (i.e., spike protein in the case of COVID-19 vaccine). Indeed, the spike is a good target for CD4+ T cell, T follicular helper (Tfh) cell, and CD8+ T cell responses in SARS-CoV-2-infected people. Correlates of protection are generally established by comparative immunological assays or studies. One of the simplest examples is from studies using neutralizing monoclonal antibodies (nMAbs). Administration of either of two human nMAbs provided rhesus macaques with sterilizing immunity to challenge(1). When administered to humans early in infection, nMAbs help prevent progression to serious disease, indicating that neutralizing antibodies are likely to be a correlate of protection. Paradoxically, however, people with severe disease tend to have very high levels of neutralizing antibodies, so it may be that the timing of the presence of sufficient antibodies is important or that the types of neutralizing antibodies matter. And, it is important to remember that a correlate of protection does not mean that the measured parameter is the sole cause of protection. Correlation is not causation. Obviously, additional complex immune mechanisms are required for protection.
A study of antibody levels in more than 12,000 health care workers exposed to SARS-CoV-2 indicated that serum antibody levels to either the spike or nucleocapsid proteins correlated with protection against infection(2). Antibody seropositivity was correlated with a nine-fold reduction in subsequent infections, and the few infections that occurred were all asymptomatic.
 Animal models provide the most convenient way to identify correlates of protection because of the ability to conduct direct viral challenge experiments. The disadvantage of animal models is that they may not accurately reflect what happens in humans. However, they do provide valuable insights. In this light, a recent report on correlates of protection in rhesus macaques(3) is of interest. Administration of purified neutralizing IgG from convalescent macaques protected from infection in a dose dependent fashion. Interestingly, depletion of CD8+ T cells prior to challenge partially abrogated protection by intermediate IgG doses. This suggests that 1) adequate titers of neutralizing antibodies are sufficient for protection; and 2) at lower doses both neutralizing antibodies and CD8-related immunity are necessary for protection, but neither is sufficient. Monoclonal neutralizing antibodies from convalescent humans showed therapeutic and prophylactic efficacy in a hamster model of infection, providing further evidence that neutralizing antibodies can play major role in protection. As mentioned above, timely administration of neutralizing antibodies to infected humans can protect against progression to severe disease. However, the efficiency of previously developed therapeutic antibodies was greatly reduced against emerging SARS-CoV-2 variants of concern containing E484K mutation.
Animal models provide the most convenient way to identify correlates of protection because of the ability to conduct direct viral challenge experiments. The disadvantage of animal models is that they may not accurately reflect what happens in humans. However, they do provide valuable insights. In this light, a recent report on correlates of protection in rhesus macaques(3) is of interest. Administration of purified neutralizing IgG from convalescent macaques protected from infection in a dose dependent fashion. Interestingly, depletion of CD8+ T cells prior to challenge partially abrogated protection by intermediate IgG doses. This suggests that 1) adequate titers of neutralizing antibodies are sufficient for protection; and 2) at lower doses both neutralizing antibodies and CD8-related immunity are necessary for protection, but neither is sufficient. Monoclonal neutralizing antibodies from convalescent humans showed therapeutic and prophylactic efficacy in a hamster model of infection, providing further evidence that neutralizing antibodies can play major role in protection. As mentioned above, timely administration of neutralizing antibodies to infected humans can protect against progression to severe disease. However, the efficiency of previously developed therapeutic antibodies was greatly reduced against emerging SARS-CoV-2 variants of concern containing E484K mutation.
If we accept neutralizing antibodies as a correlate of protection, it is important to understand what level of such antibodies are effective. This is of particular interest in both vaccinees and infected recovered people, as such antibodies wane over time. A recent study attempted to address this issue(4) by generating a statistical model from available data with vaccinees and convalescent patients to correlate in vitro neutralizing antibody titers with protection. They estimated that 20% of the average convalescent antibody level would afford 50% protection against infection and that 3% would afford 50% protection against severe infection. They suggested that by 250 days post-vaccination, waning antibody levels will result in a significant loss of protection against infection, but protection will persist against severe disease.
A study of antibody levels in more than 12,000 health care workers exposed to SARS-CoV-2 indicated that serum antibody levels to either the spike or nucleocapsid proteins correlated with protection against infection(2).
They estimated that 20% of the average convalescent antibody level would afford 50% protection against infection and that 3% would afford 50% protection against severe infection. They suggested that by 250 days post-vaccination, waning antibody levels will result in a significant loss of protection against infection, but protection will persist against severe disease.
More studies will be required for understanding the mechanisms of protective adaptive immune responses to COVID-19 as well as the duration of memory immune responses and protective immunity to SARS-CoV-2. Thus, so far, our current knowledge leaves neutralizing antibodies as the best available correlate of protection.
Taking neutralizing antibodies as a correlate of protection, what is this likely to mean about infection with variant viruses of concern? One cause for worry is the reduced efficacy of nMAbs on such variants. The South African variant, B1.351, is resistant to all three therapeutically used nMAbs, and is not neutralized by about 50% of convalescent sera(5). Another report(6) with sera from people vaccinated with either the Moderna or the Pfizer vaccine showed that neutralization activity was not affected against B1.1.7 (the UK variant); however, against B1.351, neutralization efficacy was reduced 10- to 12-fold. Reduction of neutralizing activity against other variants containing E484K mutation has also been found. Yet, despite these worrying findings it is worth noting that SARS-CoV-2-specific CD4+T cells and CD8+ T cells correlated with reduced disease severity in COVID-19 patients. Also it is unlikely that SARS-CoV-2 mutations would escape T cell immunity, because a very broad array of SARS-CoV-2 epitopes are recognized in humans with COVID-19 (7). Therefore, if we accept this as a correlate of protection, these vaccines will afford decreased protection against B1.351 infection but may still suffice to protect against serious disease.
Conclusion
One caveat about leaping to this conclusion is that we don’t know what other immune activities might play a protective role against disease, since both the Moderna and the Pfizer vaccines seem to retain protection against severe disease from B1.351. It should be emphasized that, particularly at extended times after infection or vaccination, serum antibodies may not be perfectly predictive of protection, as persistent memory B-cells and T-cells may allow the rapid reappearance of such antibodies. More studies will be required for understanding the mechanisms of protective adaptive immune responses to COVID-19 as well as the duration of memory immune responses and protective immunity to SARS-CoV-2. Thus, so far, our current knowledge leaves neutralizing antibodies as the best available correlate of protection.
- S. J. Zost et al., Potently neutralizing and protective human antibodies against SARS-CoV-2. Nature 584, 443-449 (2020).
- S. F. Lumley et al., Antibody Status and Incidence of SARS-CoV-2 Infection in Health Care Workers. N Engl J Med 384, 533-540 (2021).
- K. McMahan et al., Correlates of protection against SARS-CoV-2 in rhesus macaques. Nature 590, 630-634 (2021).
- D. S. Khoury et al., What level of neutralising antibody protects from COVID-19? medRxiv, 2021.2003.2009.21252641 (2021).
- C. K. Wibmer et al., SARS-CoV-2 501Y.V2 escapes neutralization by South African COVID-19 donor plasma. Nat Med, (2021).
- P. Wang et al., Antibody Resistance of SARS-CoV-2 Variants B.1.351 and B.1.1.7. bioRxiv, 2021.2001.2025.428137 (2021).
- Sette, A. and Crotty, S. Adaptive immunity to SARS-CoV-2 and COVID-19. Cell 184: 861-880 (2011).
