Avian Influenza Viruses
Avian Influenza Viruses
November 26, 2021
The global death toll from COVID-19 reached 5 million on November 1, 2021, but the actual figures are likely much higher (1). In recent history, the 1918 H1N1 flu pandemic caused by an Influenza A (H1N1) virus was the most severe known pandemic, killing more than 50 million people worldwide (2). The sequence analysis of the hemagglutinin (HA) gene suggested that the pandemic virus derived from an avian influenza virus immediately before 1918, possibly through a swine intermediary (3).
 Influenza A Viruses (IAVs)
Influenza A Viruses (IAVs)
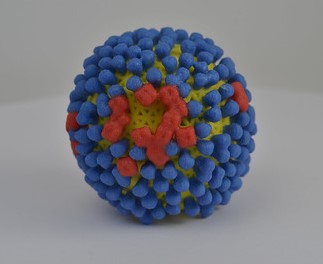
Influenza A viruses (IAVs) have been isolated from many animal species, but wild waterfowl and shorebirds are recognized as their natural reservoirs (4). The host range of IAVs is mainly determined by the affinity of HA binding to terminal sialic acids of glycoproteins on the surfaces of respiratory epithelial cells (5). Avian and human viruses preferentially bind to sialic acid linked to galactose via an α2-3 linkage (SAα2,3Gal) and galactose via an α2-6 linkage (SAα2,6Gal), respectively. The HA and NA (neuraminidase) proteins of IAV are surface glycoproteins and important for virus infectivity. The HA protein is responsible for binding to receptors on host cells, thereby initiating infection and a major target of the humoral immune response (6). The NA protein, besides also being a target for the humoral immune response, plays a role in increase and spread of progeny virions by removing sialic acid from glycoproteins. On the basis of antigenic specificity, IAV can be classified by the combination of HA (H1 to H18) and NA (N1 to N11) proteins. In particular, highly pathogenic avian influenza viruses (HPAIVs) of the H5 and H7 subtypes have evolved rapidly, thus increasing bird-to-human transmission efficacy, although subsequent human-to-human transmission is limited. Most human infections were caused by contact with infected domestic poultry or their contaminated environments. HPAIVs of the H5 and H7 subtypes cause high mortality in chickens and other terrestrial poultry, as well as sporadic human infections. Globally, from January 2003 to 28 October 2021, 863 cases of human infection with HPAI H5N1 have been reported from 18 countries (7). HPAI H7N9 emerged in China in 2017. From October 2016 to September 2017, low pathogenic avian influenza and HPAI H7N9 viruses co-circulated in Asia, resulting in 766 confirmed human infections with 288 deaths (8). Amid the ongoing pandemic, HPAI H5N6 is especially raising concerns about the risk of additional human zoonotic infections and the pandemic potential of this virus (9).
HPAI H5N6
HPAI H5N6 was first detected in poultry in Laos in 2013 and then spread to Vietnam, China, and other South Asian countries, causing numerous cases in these areas (10). The increasing genetic diversity (subclades 2.3.4.4 a to 2.3.4.4 h) and geographical distribution of H5N6 pose a serious threat to the poultry industry and human health. The first case of human infection was reported in China in 2014. As of October 29, 2021, a total of 51 laboratory-confirmed cases of human infection with the virus, including 25 deaths, have been reported to WHO. China has reported 21 human infections with H5N6 in 2021. The outbreaks have resulted in at least six deaths and left many of the remaining infected people critically ill. Strikingly, the number of cases this year doubled the total number of cases detected since the first case of human infection in 2014.
In recent history, the 1918 H1N1 flu pandemic caused by an Influenza A (H1N1) virus was the most severe known pandemic, killing more than 50 million people worldwide (2).
From October 2016 to September 2017, low pathogenic avian influenza and HPAI H7N9 viruses co-circulated in Asia, resulting in 766 confirmed human infections with 288 deaths (8).
So far, most of those infected with the HPAI H5N6 virus had been in contact with domestic poultry. There were no confirmed cases of human-to-human virus spread.
A One Health approach will be critical, with genomic surveillance programs for monitoring the evolution of H5N6 and other emerging HPAIVs in wild birds, poultry, mammals, and their environments.
HPAI H5N6 Spread
So far, most of those infected with the HPAI H5N6 virus had been in contact with domestic poultry. There were no confirmed cases of human-to-human virus spread. Interestingly, H5N6 viruses isolated from waterfowl have shown to maintain the affinity for avian-like SAα2,3Gal receptors and acquired an affinity for the human-like receptor to bind human tracheal epithelial and alveolar cells, with the ensuing ability for in-contact transmission in ferrets (11). H5N6 isolated from a patient in 2014 possessed the E627K substitution in the PB2 protein, leading to mammalian adaption of avian influenza viruses (12). The virus replicated to high titers in the respiratory tracts of ferrets and caused severe pneumonia. However, the risk from airborne spread is currently considered to be low.
 Genetic Sequencing of H5N6
Genetic Sequencing of H5N6
Genetic sequence analysis of H5N6 from human cases in 2021 showed mutations in HA and other viral proteins, such as polymerase basic 1, polymerase acid, matrix 1, nonstructural 1 proteins (13). In the HA protein, the receptor-binding site at the 222–224 showed the preference of binding to avian-like receptors (SAα2,3Gal). However, other mutations found in the HA protein, including the receptor binding site, could increase viral binding to human-like receptors (SAα2,6Gal). Another study with five independent cases in 2021 also demonstrated that H5N6 is continuously evolving as a result from genomic reassortments with other subtype of avian influenza viruses (14). Therefore, considering the genetic diversity and evolution, further extensive characterization and risk assessment of different genotypes of H5N6 viruses will be required.
H5N6 Infection in Mammals
In addition to human infection with H5N6, avian influenza viruses have caused numerous other mammalian infections. For example, in spring 2014, increased mortality of harbor seals (Phoca vitulina), associated with infection with an influenza A(H10N7) virus, was reported in Sweden, Denmark, and Germany (15). Genetic sequencing analysis found the majority of sequence variation occurred in the HA gene of isolates from seals, suggesting adaptation of the virus to its new mammalian host. The seal A/H10N7 virus was aerosol or respiratory droplet transmissible between ferrets. Compared with avian H10 hemagglutinin, seal H10 hemagglutinin showed stronger binding to the human-type sialic acid receptor, with preferential binding to α2,6-linked sialic acids on long extended branches (16). In addition, various outbreaks of for H3N8, H7N7, and H4N6 low pathogenic avian influenza viruses have occurred in harbor seals along the New England coast of the United States (17). Recent studies also showed that HPAI H5N8 infected gray seals (Halichoerus grypus) stranded on the Baltic coast of Poland (18) and harbor seals at the German North Sea coast (19).
Conclusion
Avian influenza viruses, including HPAIVs, have been widely detected in wild birds and domestic poultry in many countries. Wild birds have been shown to carry and spread avian influenza viruses globally during their migratory season. For effective prevention, a One Health approach will be critical, with genomic surveillance programs for monitoring the evolution of H5N6 and other emerging HPAIVs in wild birds, poultry, mammals, and their environments. Importantly, identification of avian-origin influenza viruses across mammals appears critical to detect influenza A viruses posing a major threat to humans and other mammals.
Our GVN team thanks Dr. Albert Osterhaus (The Research Center for Emerging Infections and Zoonoses, Hannover, Germany)for reviewing this manuscript and for providing us with invaluable comments and insights.
References
- WHO Coronavirus (COVID-19) Dashboard. https://covid19.who.int.
- 1918 Pandemic (H1N1 virus) – Influenza (Flu). https://www.cdc.gov/flu/pandemic-resources/1918-pandemic-h1n1.html
- Reid, A.H., Fanning, T.G., Hultin, J.V. & Taubenberger, J.K. Origin and evolution of the 1918 “Spanish” influenza virus hemagglutinin gene. Natl. Acad. Sci. USA96, 1651– 1656 (1999).
- Sonnberg, S.; Webby, R.J.; Webster, R.G. Natural history of highly pathogenic avian influenza H5N1. Virus Res. 2013, 178, 63-77.
- Neumann, G.; Kawaoka, Y. Host range restriction and pathogenicity in the context of influenza pandemic. Emerg. Infect. Dis. 2006, 12, 881–886.
- Palese, P.; Shaw, M.L. Orthomyxoviridae: the viruses and their replication. D.M. Knipe, P.M. Howley (Eds.), Fields Virology (5th ed.), Lippincott Williams & Wilkins 2007, 1647–1689.
- Human infection with avian influenza A(H5) viruses. https://www.who.int/docs/default-source/wpro—documents/emergency/surveillance/avian-influenza/ai-20210122.pdf.
- Radvak, P., Kosikova, M., Kuo, YC. et al.Highly pathogenic avian influenza A/Guangdong/17SF003/2016 is immunogenic and induces cross-protection against antigenically divergent H7N9 viruses. npj Vaccines 6, 30 (2021). https://doi.org/10.1038/s41541-021-00295-7
- CDC Update on A(H5N6) Bird Flu: How is the U.S. CDC Monitoring A(H5N6) Infections and Contributing to Global Pandemic Preparedness? https://www.cdc.gov/flu/spotlights/2021-2022/H5N6.htm
- Li Y, Li M, Li Y, Tian J, Bai X, Yang C, et al. Outbreaks of highly pathogenic avian influenza (H5N6) virus subclade 2.3.4.4h in swans, Xinjiang, Western China, 2020. Emerg Infect Dis. 2020;26(12):2956-2960. https://doi.org/10.3201/eid2612.201201
- Sun H, Pu J, Wei Y, Sun Y, Hu J, Liu L, Xu G, Gao W, Li C, Zhang X, Huang Y, Chang KC, Liu X, Liu J. Highly Pathogenic Avian Influenza H5N6 Viruses Exhibit Enhanced Affinity for Human Type Sialic Acid Receptor and In-Contact Transmission in Model Ferrets. J Virol. 2016 Jun 24;90(14):6235-6243. doi: 10.1128/JVI.00127-16. PMID: 27122581; PMCID: PMC4936137.
- Herfst S, Mok CKP, van den Brand JMA, van der Vliet S, Rosu ME, Spronken MI, Yang Z, de Meulder D, Lexmond P, Bestebroer TM, Peiris JSM, Fouchier RAM, Richard M. Human Clade 2.3.4.4 A/H5N6 Influenza Virus Lacks Mammalian Adaptation Markers and Does Not Transmit via the Airborne Route between Ferrets. mSphere. 2018 Jan 3;3(1):e00405-17. doi: 10.1128/mSphere.00405-17. PMID: 29299528; PMCID: PMC5750386.
- Bi F, Jiang L, Huang L, Wei J, Pan X, Ju Y, Mo J, Chen M, Kang N, Tan Y, Li Y, Wang J. Genetic characterization of two human cases infected with the avian influenza A (H5N6) viruses – Guangxi Zhuang Autonomous Region, China, 2021. China CDC Wkly. 2021 Oct 29;3(44):923-928. doi: 10.46234/ccdcw2021.199. PMID: 34745693; PMCID: PMC8563334.
- Xiao C, Xu J, Lan Y, Huang Z, Zhou L, Guo Y, Li X, Yang L, Gao GF, Wang D, Liu WJ, Zhou X, Yang H. Five Independent Cases of Human Infection with Avian Influenza H5N6 – Sichuan Province, China, 2021. China CDC Wkly. 2021 Sep 3;3(36):751-756. doi: 10.46234/ccdcw2021.187. PMID: 34594983; PMCID: PMC8427102.
- Bodewes R, Zohari S, Krog JS, Hall MD, Harder TC, Bestebroer TM, van de Bildt MWG, Spronken MI, Larsen LE, Siebert U, Wohlsein P, Puff C, Seehusen F, Baumgärtner W, Härkönen T, Smits SL, Herfst S, Osterhaus ADME, Fouchier RAM, Koopmans MP, Kuiken T. Spatiotemporal Analysis of the Genetic Diversity of Seal Influenza A(H10N7) Virus, Northwestern Europe. J Virol. 2016 Apr 14;90(9):4269-4277. doi: 10.1128/JVI.03046-15. PMID: 26819311; PMCID: PMC4836327.
- Herfst S, Zhang J, Richard M, McBride R, Lexmond P, Bestebroer TM, Spronken MIJ, de Meulder D, van den Brand JM, Rosu ME, Martin SR, Gamblin SJ, Xiong X, Peng W, Bodewes R, van der Vries E, Osterhaus ADME, Paulson JC, Skehel JJ, Fouchier RAM. Hemagglutinin Traits Determine Transmission of Avian A/H10N7 Influenza Virus between Mammals. Cell Host Microbe. 2020 Oct 7;28(4):602-613.e7. doi: 10.1016/j.chom.2020.08.011. PMID: 33031770; PMCID: PMC7556738.
- Short KR, Richard M, Verhagen JH, van Riel D, Schrauwen EJ, van den Brand JM, Mänz B, Bodewes R, Herfst S. One health, multiple challenges: The inter-species transmission of influenza A virus. One Health. 2015 Dec 1;1:1-13. doi: 10.1016/j.onehlt.2015.03.001. PMID: 26309905; PMCID: PMC4542011.
- Shin DL, Siebert U, Lakemeyer J, et al. Highly Pathogenic Avian Influenza A(H5N8) Virus in Gray Seals, Baltic Sea. Emerg Infect Dis. 2019;25(12):2295-2298. doi:10.3201/eid2512.181472.
- Postel A. et al. Infections with highly pathogenic avian influenza A virus (HPAIV) H5N8 in harbor seals at the German North Sea coast, 2021 (submitted).
