Does COVID-19 Curb or Promote the Progression of Cancer?
Does COVID-19 Curb or Promote the Progression of Cancer?
July 2, 2021
 One of the many questions about the long-term implications of COVID-19 is whether there might be some positive or negative consequences on cancer. The inflammatory milieu elicited by infection with SARS-CoV-2 might elicit pro-cancer effects as well as COVID-related immune-deficiency or increase DNA damage through the activity of reactive oxygen species along with the p53 oncosuppressor inactivation by the SARS-CoV-2 NSP3 and NSP2 nonstructural proteins (1). In contrast, infection by SARS-CoV-2 could conceivably yield anti-cancer effects. In fact, some viruses have been used as oncolytic agents by selectively killing cancer cells. In some other cases, stimulation of innate immunity might result in triggering immune responses to cancer cells. Neither possibility is mutually exclusive.
One of the many questions about the long-term implications of COVID-19 is whether there might be some positive or negative consequences on cancer. The inflammatory milieu elicited by infection with SARS-CoV-2 might elicit pro-cancer effects as well as COVID-related immune-deficiency or increase DNA damage through the activity of reactive oxygen species along with the p53 oncosuppressor inactivation by the SARS-CoV-2 NSP3 and NSP2 nonstructural proteins (1). In contrast, infection by SARS-CoV-2 could conceivably yield anti-cancer effects. In fact, some viruses have been used as oncolytic agents by selectively killing cancer cells. In some other cases, stimulation of innate immunity might result in triggering immune responses to cancer cells. Neither possibility is mutually exclusive.
Current Data
With respect to whether COVID-19 might cause an increase in cancer, the answers will have to await the passage of time. Current clinical/epidemiological data do not provide evidence for this possibility. On the other hand, regarding a hypothetical possibility of an anti-cancer effect, there are some theoretical considerations and some anecdotal data indicating that innate immunity might have a cross-protective effect or that the virus might have oncolytic activity. We wish to emphasize that they are still very preliminary; yet in this perspective, we have reviewed those reports.
Effects on Metastatic Colorectal Cancer (mCRC)
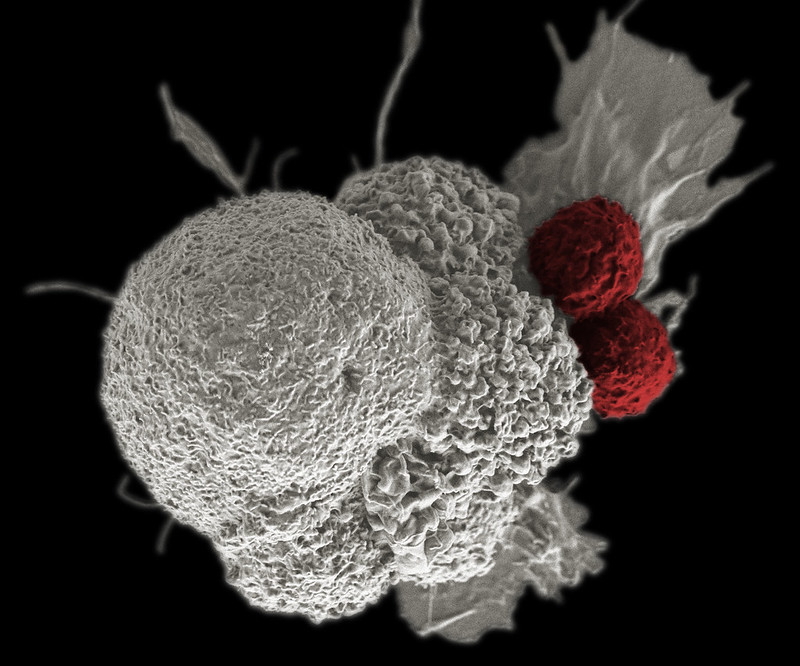
One of the more compelling reports involved a small cohort of metastatic colorectal cancer (mCRC) patients (2). Three mCRC patients became infected with SARS-CoV-2. During their infection, all three experienced reductions of their disease burden, as judged by radiologic imaging. One patient developed severe COVID-19, from which he recovered. During this time, there was a complete regression of his hepatic metastases. A second mCRC patient developed mild COVID-19. Similar to the first patient, he experienced resolution of several of his hepatic metastases. The third patient developed mild symptomatic COVID-19. Following this, she experienced unexpected reductions in peritoneal and lung lesions, as judged by CT scans. All three patients developed IgG titers against SARS-CoV-2 that varied between 188 U/ml and 1455 U/ml by electrochemiluminescence assays, indicating an adaptive immune response to the virus. This report is largely anecdotal; however, it is interesting to note that the four other mCRC patients in the same cohort did not show cancer reduction and showed IgG from low to undetectable levels against SARS-CoV-2. This suggests that antitumor activity due to viral infection would require an active immune response to the virus, either by induction of innate immunity or a heterogenous response to infection. It may be that the non-responding mCRC patients were immune deficient from their cancers.
In contrast, infection by SARS-CoV-2 could conceivably yield anti-cancer effects. In fact, some viruses have been used as oncolytic agents by selectively killing cancer cells.
One patient developed severe COVID-19, from which he recovered. During this time, there was a complete regression of his hepatic metastases. A second mCRC patient developed mild COVID-19. Similar to the first patient, he experienced resolution of several of his hepatic metastases
These reports, although limited, suggest that infection with SARS-CoV-2 might conceivably trigger an anti-tumor immune response. The results, although anecdotal, are suggestive and intriguing; thus, they should stimulate further research in this area.
Epstein-Barr Virus (EBV)-Associated Lymphoma
Another report is of a patient with a treatment-refractory natural killer (NK)/T-cell Epstein–Barr virus (EBV)-associated lymphoma who experienced transient and partial but distinct remission upon infection with SARS-CoV-2 (3). The clonal neoplastic NK cell population dropped from 70% to 4%, and EBV DNA titers dropped from about 230,000 copies/ml to about 500 copies/ml. Splenomegaly also decreased. However, after resolution of COVID-19, there was a rapid return of EBV DNA titers to 72,000, NK cell numbers, and splenomegaly. The authors speculate that SARS-CoV-2 may have caused the drop in NK cell titers by an immunomodulatory activity and note that COVID-19 is generally associated with reduced amounts of NK cells, probably due to over-expression of inflammatory cytokines.
 Hodgkin’s Disease
Hodgkin’s Disease
In addition, another report describes the case of a patient with Hodgkin’s disease (4). The patient was diagnosed by lymph node biopsy, with an EBV DNA titer of 4,800 copies/ml. Shortly thereafter, he was diagnosed with PCR-positive COVID-19. After 11 days of supportive care, he was sent home to convalesce. Four months later, there was a marked reduction of lymphadenopathy and a reduction in EBV titers to 413 copies/ml. The authors speculate that COVID-19 triggered an anti- tumor immune response, similar to what has been reported for other infections in a setting of high-grade non-Hodgkin’s lymphoma (5). Further follow-up of the patient was not reported.
Conclusion
Clearly, these reports, although limited, suggest that infection with SARS-CoV-2 might conceivably trigger an anti-tumor immune response. The results, although anecdotal, are suggestive and intriguing; thus, they should stimulate further research in this area.
Acknowledgment
- Cardozo CM and Hainaut P., Viral strategies for circumventing p53: the case of severe acute respiratory syndrome coronavirus. Curr Opin Oncol. 2021 Mar 1;33(2):149-158. doi: 10.1097/CCO.0000000000000713. PMID: 33405482; PMCID: PMC7924916
- Ottaiano et al., Unexpected tumor reduction in metastatic colorectal cancer patients during SARS-Cov-2 infection. Therapeutic Advances in Medical Oncology 13, 17588359211011455 (2021).
- Pasin et al., Oncolytic effect of SARS-CoV2 in a patient with NK lymphoma. Acta Biomed 91, ahead of print (2020).
- Challenor, D. Tucker, SARS-CoV-2-induced remission of Hodgkin lymphoma. British Journal of Haematology 192, 415-415 (2021).
- W. Buckner et al., Complete spontaneous remission of diffuse large B-cell lymphoma of the maxillary sinus after concurrent infections. Clin Lymphoma Myeloma Leuk 12, 455-458 (2012).
