COVID-19 and Autoimmunity
COVID-19 and Autoimmunity
Are Severe Cases of COVID-19 Related to an Autoimmune Disease?
February 15, 2021
COVID-19, the disease caused by SARS-CoV-2, involves at least two distinct phases. The first phase is attributed to typical progress of respiratory disease by causing fever, cough, loss of taste/smell, and other symptoms typical of respiratory infections. The second phase, which occurs less frequently, is more serious and can include a great variety of multi-organ manifestations, including lung, heart, vasculature, and central nervous system. For more detail, please see the previous Perspective on COVID-19 Long Haulers (https://gvn.org/what-does-it-mean-to-be-a-covid-19-long-hauler/). It is important to note that the vast majority of infected people do not experience severe disease in the first place.
We will consider evidence that the latter stage of COVID-19 associates with autoimmunity. It should be pointed out that autoimmune phenomena falls into two categories: (1) the innate immune system activates adaptive B- or T-cell-mediated immune responses that lead to damaging inflammation (autoimmunity) and (2) the innate immune system causes inflammatory damage directly (autoinflammatory). In both cases, the innate immune system is intimately involved, and mostly, there is a spectrum of these patterns. It should also be noted that it can be difficult to clearly discriminate between functional and dysfunctional immune responses without an understanding of the specific correlates of protection. We will not consider situations in which autoimmunity exists prior to infection, as in the case of patients with pre-existing autoantibodies to type 1 interferons(1). Interestingly, some individuals have pre-existing stereotypic SARS-CoV-2 neutralizing antibodies, produced by naïve B cells, without any known case of viral exposure(2).
Autoantibodies
In this GVN Perspective, we will first focus on autoimmunity mediated by autoantibodies. One mechanism of autoimmunity is by molecular mimicry(3), in which a viral protein sequence resembles a cellular protein sequence. Thus, the elicited antibodies target not only the viral protein but also the related cellular proteins. The region of similarity need not be large; a stretch of a dozen or so closely related amino acid residues can result in molecular mimicry. Specifically, overlapping hexa- and heptapeptides spanning the SARS-CoV-2 spike protein were found to be homologous to a large number of peptides in the human proteome(4). This does not necessarily establish a basis for autoimmunity. However, other studies show the presence of many different autoantibodies in COVID-19 patients. We will describe these findings in detail. We acknowledge that there are many other cases. In addition, low levels of autoreactivity are common, and these did not generally manifest symptomatically.
Autoantibodies and COVID-19
High levels of autoantibodies against Annexin A2 were shown to elevate above average in hospitalized COVID-19 patients (5). Higher levels of autoantibodies were predictive of mortality, with an odds ratio of 9.3. Annexin A2 (a phospholipid-binding protein) that is involved in cell membrane stabilization, fibrinolysis, and stability of the microvasculature. It is not a great leap of imagination to link this with clotting disorders and microvascular issues, which are commonly found in severe cases of COVID-19 patients. Similarly, half of hospitalized COVID-19 patients had at least 1 of 8 measured anti-phospholipid antibodies (6), and these levels correlated with activation of coagulation pathways, including release of neutrophil extracellular traps and elevated platelet levels. Furthermore, when these antibodies were purified and injected into mice, they caused accelerated coagulation in mice.
Interestingly, some individuals have pre-existing stereotypic SARS-CoV-2 neutralizing antibodies, produced by naïve B cells, without any known case of viral exposure(2).
High levels of autoantibodies against Annexin A2 were shown to elevate above average in hospitalized COVID-19 patients (5). Higher levels of autoantibodies were predictive of mortality, with an odds ratio of 9.3.
In addition to autoantibodies, T cell activation can play a role in autoimmunity. The spike protein of SARS-CoV-2 contains a high affinity motif for binding T cell receptors.
Autoimmune phenomena are likely an intimate aspect of the pathogenesis of COVID-19. Indeed, the use of corticosteroids has proven to be an effective treatment for latter stage of COVID-19.
A variety of other autoantibodies have shown to be associated with severe cases of COVID-19 (7-9). Bhadelia et al.(7) showed that 5/5 individuals with persistent symptoms and 2/4 without persistent symptoms had autoantibodies that included anti-β2 glycoprotein, -proteinase 3-ANCA, -MI-2, and -PM1/SCL-100, suggesting their potential role in long-term COVID-19. Many of the identified activities are associated in non-COVID-19 individuals with vasculitis, myelopathies, and anti-phospholipid syndromes. COVID-19 patients had autoantibodies to chemokines, cytokines, complement components and cell surface proteins, including type 1 interferons and chemokine receptors, which can affect immune function (8). Woodruff et al.(9) found elevated levels of anti-nuclear antibodies in severe COVID-19 patients. The presence of autoantibodies may be correlated with extrafollicular B cell activation pathways, which also correlate with neutralizing antibody production (10).
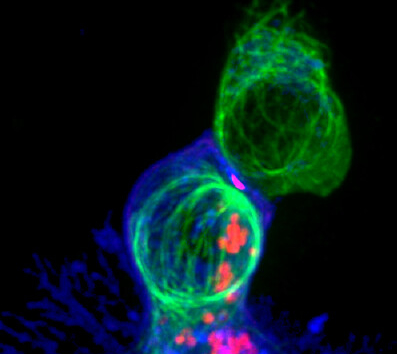
T-Cell Activation and Innate Immunity
In addition to autoantibodies, T cell activation can play a role in autoimmunity. The spike protein of SARS-CoV-2 contains a high affinity motif for binding T cell receptors. This is very similar to staphylococcal enterotoxin B(11), a superantigen, that is responsible for cytokine storm induction. This might result in high viral titers causing massive cytokine expression, which perhaps could persist after viral clearance.
Another study evaluated the effects of manipulation of innate immunity by SARS-CoV-2(12). Viral Infection inhibited activation of the interferon arm of the innate immune system, but does not block activation of the inflammatory cytokine arm, thus allowing excessive expression of IL-6 and various chemokines. This might serve as the driving force behind severe cases of COVID-19. Persistence of the inflammatory state is in effect an autoinflammatory state.
Conclusion
Autoimmune phenomena are likely an intimate aspect of the pathogenesis of COVID-19. Indeed, the use of corticosteroids has proven to be an effective treatment for latter stage of COVID-19. We need a significantly better understanding of the mechanisms by which SARS-CoV-2 influences innate immunity and type 1 interferon expression and activity to deal effectively with severe cases of COVID-19.
- P. ####### et al., Auto-antibodies against type I IFNs in patients with life-threatening COVID-19. Science, (2020).
- S. I. Kim et al., Stereotypic neutralizing VH antibodies against SARS-CoV-2 spike protein receptor binding domain in patients with COVID-19 and healthy individuals. Science Translational Medicine 13, eabd6990 (2021).
- M. B. A. Oldstone, Molecular Mimicry: Its Evolution from Concept to Mechanism as a Cause of Autoimmune Diseases. Monoclonal Antibodies in Immunodiagnosis and Immunotherapy 33, 158-165 (2014).
- D. Kanduc, Y. Shoenfeld, Molecular mimicry between SARS-CoV-2 spike glycoprotein and mammalian proteomes: implications for the vaccine. Immunologic Research 68, 310-313 (2020).
- M. Zuniga et al., Autoimmunity to the Lung Protective Phospholipid-Binding Protein Annexin A2 Predicts Mortality Among Hospitalized COVID-19 Patients. medRxiv, 2020.2012.2028.20248807 (2021).
- Y. Zuo et al., Prothrombotic autoantibodies in serum from patients hospitalized with COVID-19. Sci Transl Med 12, (2020).
- N. Bhadelia et al., Distinct Autoimmune Antibody Signatures Between Hospitalized Acute COVID-19 Patients, SARS-CoV-2 Convalescent Individuals, and Unexposed Pre-Pandemic Controls. medRxiv, 2021.2001.2021.21249176 (2021).
- E. Y. Wang et al., Diverse Functional Autoantibodies in Patients with COVID-19. medRxiv, 2020.2012.2010.20247205 (2020).
- M. C. Woodruff, R. P. Ramonell, F. E.-H. Lee, I. Sanz, Clinically identifiable autoreactivity is common in severe SARS-CoV-2 Infection. medRxiv, 2020.2010.2021.20216192 (2020).
- M. C. Woodruff et al., Extrafollicular B cell responses correlate with neutralizing antibodies and morbidity in COVID-19. Nat Immunol 21, 1506-1516 (2020).
- M. H. Cheng et al., Superantigenic character of an insert unique to SARS-CoV-2 spike supported by skewed TCR repertoire in patients with hyperinflammation. Proc Natl Acad Sci U S A 117, 25254-25262 (2020).
- D. Blanco-Melo et al., Imbalanced Host Response to SARS-CoV-2 Drives Development of COVID-19. Cell 181, 1036-1045 e1039 (2020).
