Resurgent Outbreaks of Measles
Resurgent Outbreaks of Measles
May 18, 2022
 Introduction
Introduction
Two years of the COVID-19 pandemic has brought another health crisis to children. The number of measles cases reported worldwide (more than 17,300 cases) has increased by 79 percent in the first two months of 2022 compared to the same time last year (1). Countries with the largest measles outbreaks in the past year include Afghanistan, Ethiopia, Nigeria, Somalia and Yemen. Measles can be prevented by effective immunization. In fact, the WHO reported that between 2000 and 2017, MV vaccines have prevented more than 21 million deaths directly attributable to measles (2). However, the pandemic interrupted vaccination campaigns for children. WHO and UNICEF are warning that an increase in measles cases is a worrying sign of a heightened risk for the spread of vaccine-preventable diseases and could trigger larger outbreaks (3). As measles is highly contagious, cases tend to show up quickly when vaccination levels decline. Pandemic-related disruptions, increasing inequalities in access to vaccines, and the diversion of resources from routine immunization are leaving too many children without protection against measles and other vaccine-preventable diseases. In general, coverage at or above 95% with 2 doses of the safe and effective measles vaccine can protect children against measles and eliminate endemic virus transmission. However, COVID-19 pandemic related disruptions have delayed the introduction of the second dose of the measles vaccine in many countries.
Transmission and Symptoms
Measles spreads through airborne transmission (4). Measles remains one of the most significant causes of child morbidity and mortality worldwide with the greatest burden in the youngest children (younger than 5 years of age) (5). Common measles complications include ear infections and diarrhea (4). Some people may suffer from severe complications, such as pneumonia (infection of the lungs) and encephalitis (swelling of the brain). They may need to be hospitalized and can die. Subacute sclerosing panencephalitis (SSPE) is a very rare, but fatal disease of the central nervous system that results from a measles virus infection acquired earlier in life. SSPE generally develops 7 to 10 years after a person has measles, even though the person seems to have fully recovered from the illness. While vaccination has drastically reduced global measles deaths (a 73% drop between 2000-2018 worldwide), measles is still common in many developing countries, particularly in parts of Africa and Asia (4). More than 140,000 people died from measles in 2018. The overwhelming majority (more than 95%) of measles deaths occur in countries with low per capita incomes and weak health infrastructures.
The number of measles cases reported worldwide (more than 17,300 cases) has increased by 79 percent in the first two months of 2022 compared to the same time last year (1).
While vaccination has drastically reduced global measles deaths (a 73% drop between 2000-2018 worldwide), measles is still common in many developing countries, particularly in parts of Africa and Asia (4). More than 140,000 people died from measles in 2018.
The findings of this study showed that measles virus infection causes changes in naïve and memory B lymphocyte diversity that persist after the resolution of clinical disease, and thus contribute to compromised immunity to previous infections or vaccinations.
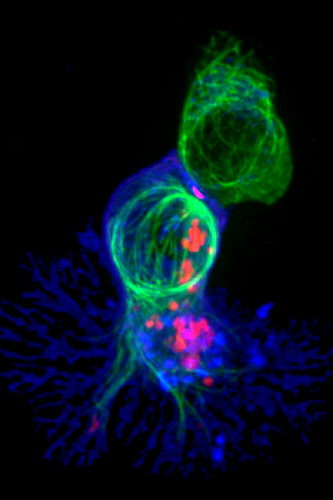
Measles is an acute systemic viral infection that targets immune cells, resulting in both viremia and lymphopenia (6). Measles virus infection does not induce type 1 interferons, but leads to production of cytokines and chemokines. This restricted response allows extensive virus replication and spread during a clinically silent latent period of 10-14 days. During acute infection, the rash marks the appearance of the adaptive immune response and clearance of infectious virus (7). Clearance of viral RNA from blood and tissues is slower and occurs over weeks to months after resolution of the rash. In particular, viral RNA persists in lymphoid tissue accompanied by ongoing germinal center proliferation, production of antibody-secreting cells, functionally distinct populations of T cells and antibody avidity maturation to establish life-long immunity (8). At the same time, diversity of pre-existing antibodies and numbers of memory and naive B cells are reduced and susceptibility to other infections is increased.
 Immune Response
Immune Response
To identify and quantify long-term effects of measles on the immune system, a clinical study was conducted to track antibodies to thousands of pathogen epitopes in blood (9). This study investigated 77 unvaccinated children before and 2 months after natural measles virus infection. Measles caused elimination of 11 to 73% of the antibody repertoire across individuals. Notably, these immune system effects were not observed in infants vaccinated with MMR (measles, mumps, and rubella), but were confirmed in measles virus-infected macaques. The reduction in humoral immune memory after measles generates potential vulnerability to future infections. In fact, use of B cell receptor (BCR) sequencing of human peripheral blood lymphocytes before and after MV infection led to the identification of two immunological consequences from measles underlying immunosuppression: (i) incomplete reconstitution of the naïve B cell pool leading to immunological immaturity and (ii) compromised immune memory to previously encountered pathogens due to depletion of previously expanded B memory clones (10). Using a surrogate model of measles in ferrets, this study further investigated the clinical consequences of viral infection and demonstrated a depletion of vaccine-acquired immunity to influenza virus, leading to a compromised immune recall response and increased disease severity after secondary influenza virus challenge. The findings of this study showed that measles virus infection causes changes in naïve and memory B lymphocyte diversity that persist after the resolution of clinical disease, and thus contribute to compromised immunity to previous infections or vaccinations. These studies highlight the importance of measles vaccination, not only for the control of measles, but also for the maintenance of herd immunity to other pathogens.
Conclusion
The current outbreak figures are likely higher due to disruptions in global surveillance systems caused by the ongoing COVID-19 pandemic. Approximately 73 million children are at risk of measles due to missed vaccinations. Furthermore, current cases mostly occur in Africa and the East Mediterranean regions that have faced social and economic hardships due to COVID-19, conflict, or other crises. They also have chronically weak health system infrastructure and insecurity. It is urgent for these countries to implement plans to prevent and respond to outbreaks of vaccine-preventable diseases and to strengthening immunization systems as part of COVID-19 recovery efforts (3).
The GVN Team thanks Dr. Diane Griffin (The Johns Hopkins Bloomberg School of Public Health) for reviewing this manuscript and for providing us with invaluable comments and insights.
References
- Measles cases are spiking globally. https://www.unicef.org/stories/measles-cases-spiking-globally
- Measles fact sheet (2019); www.who.int/news-room/fact-sheets/detail/measles.
- UNICEF and WHO warn of perfect storm of conditions for measles outbreaks, affecting children. https://www.who.int/news/item/27-04-2022-unicef-and-who-warn-of–perfect-storm–of-conditions-for-measles-outbreaks–affecting-children
- Measles. https://www.cdc.gov/globalhealth/newsroom/topics/measles/index.html
- . https://www.who.int/health-topics/measles#tab=tab_1
- Griffin DE, Lin WH, Pan CH. Measles virus, immune control, and persistence. FEMS Microbiol Rev. 2012 May;36(3):649-62. doi: 10.1111/j.1574-6976.2012.00330.x. Epub 2012 Mar 13. PMID: 22316382; PMCID: PMC3319515.
- Griffin DE. The Immune Response in Measles: Virus Control, Clearance and Protective Immunity. Viruses. 2016 Oct 12;8(10):282. doi: 10.3390/v8100282. PMID: 27754341; PMCID: PMC5086614.
- Griffin DE. Measles immunity and immunosuppression. Curr Opin Virol. 2021 Feb;46:9-14. doi: 10.1016/j.coviro.2020.08.002. Epub 2020 Sep 4. PMID: 32891958; PMCID: PMC7994291.
- Mina MJ, Kula T, Leng Y, Li M, de Vries RD, Knip M, Siljander H, Rewers M, Choy DF, Wilson MS, Larman HB, Nelson AN, Griffin DE, de Swart RL, Elledge SJ. Measles virus infection diminishes preexisting antibodies that offer protection from other pathogens. Science. 2019 Nov 1;366(6465):599-606. doi: 10.1126/science.aay6485. PMID: 31672891; PMCID: PMC8590458.
- Petrova VN, Sawatsky B, Han AX, Laksono BM, Walz L, Parker E, Pieper K, Anderson CA, de Vries RD, Lanzavecchia A, Kellam P, von Messling V, de Swart RL, Russell CA. Incomplete genetic reconstitution of B cell pools contributes to prolonged immunosuppression after measles. Sci Immunol. 2019 Nov 1;4(41):eaay6125. doi: 10.1126/sciimmunol.aay6125. PMID: 31672862.
